Understanding Laser Assisted In Situ Keratomileusis

Intro
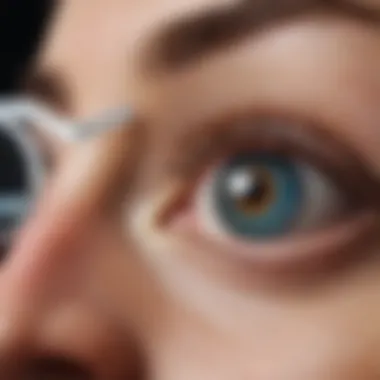
Laser Assisted In Situ Keratomileusis, commonly known as LASIK, has transformed the field of refractive eye surgery. This procedure allows for the correction of a variety of visual impairments, providing patients with a remarkable alternative to glasses and contact lenses. Understanding LASIK involves exploring its principles, methodology, benefits, risks, and post-operative considerations.
In this article, we aim to dissect the technicalities of LASIK, delve into patient experiences, and examine how advancements in technology continue to shape this surgical procedure.
Research Overview
Summary of Key Findings
Recent studies illustrate that LASIK can effectively rectify near-sightedness, far-sightedness, and astigmatism. The surgery offers benefits such as rapid recovery time and improved visual acuity. However, it is essential to recognize potential complications.
- High satisfaction rates: Many patients report significant improvements in their vision.
- Quick recovery: Most individuals notice improved sight within a day.
- Risks: While rare, complications like dry eyes and glare are possible.
Background and Context
The origin of LASIK can be traced back to the 1980s, evolving from earlier surgical techniques. The introduction of the excimer laser marked a significant shift, allowing for precision in the reshaping of corneal tissue. Over time, enhancements have been made in the tools and methods employed.
Methodology
Experimental Design
LASIK procedures are conducted in a controlled clinical environment. The surgery involves two primary steps: creating a thin flap in the cornea and then reshaping the underlying tissue with a laser. This design ensures minimal invasiveness and facilitates quick recovery.
Data Collection Techniques
Data on LASIK outcomes is collected through patient surveys and clinical evaluations post-surgery. Outcomes are often measured through visual acuity tests and patient-reported satisfaction levels.
"Understanding the nuances of LASIK is crucial for both potential candidates and healthcare professionals. Awareness of the process can lead to informed decisions and optimal results."
The complexities of LASIK encompass both scientific principles and the human element, painting a comprehensive picture of this widely adopted refractive surgery.
Preface to LASIK
Laser Assisted In Situ Keratomileusis, commonly referred to as LASIK, is a surgical procedure that holds a significant position within refractive eye surgery. This article aims to consolidate the essential concepts surrounding LASIK, exploring its development, operation, and impact on visual health. Understanding LASIK is crucial for students, researchers, educators, and professionals who wish to grasp the nuances of modern eye surgery.
LASIK has transformed how we approach visual impairments, offering a non-invasive option with promising results. As refractive surgery continues to evolve, so too do the techniques and technologies behind LASIK. Evolving patient needs and increasing cases of refractive errors drive the urgency to understand this field deeply. It is important to consider the criteria for patient selection, preoperative assessments, and postoperative care as part of LASIK's comprehensive narrative.
In exploring LASIK, we will dissect its history and development, providing context to its current applications. The goal is for readers to fully appreciate how LASIK can improve life quality while also acknowledging associated risks. The subsequent sections will break down LASIK further, allowing for a clear grasp of its intricacies.
The Evolution of Refractive Surgery
Refractive surgery began evolving over decades — from rudimentary techniques to the sophisticated methods we have today. Early attempts, such as radial keratotomy, laid the foundation for what would become an entire field dedicated to correcting vision. The innovations brought forth by laser technology marked a turning point in refractive surgery.
In the 1990s, LASIK emerged as a prominent option, making use of the excimer laser. The advent of this technology enabled surgeons to reshape the cornea with precision, allowing for better outcomes and reduced recovery times. This contributes to LASIK’s reputation as a desirable procedure among patients worldwide.
More recent developments include advanced wavefront technology, providing tailored treatments for individual corneal abnormalities. The path of refractive surgery shows a relentless pursuit of improving patient experience and outcomes.
Defining Laser Assisted In Situ Keratomileusis
Laser Assisted In Situ Keratomileusis is a method designed to correct common vision problems such as myopia, hyperopia, and astigmatism. The acronym LASIK encapsulates the essential elements of the procedure. In essence, it involves reshaping the cornea using a laser to optimize its focusing capacity.
During LASIK, the surgeon first creates a thin flap in the cornea, which is then lifted. An excimer laser reshapes the underlying corneal tissue. Once the necessary alterations are made, the flap is repositioned, often without the need for sutures. This process is both quick and minimally invasive, leading to swift recovery.
The precision of the laser technology is key in this process, allowing adjustments to be made with microscale accuracy. LASIK aims to reduce dependence on glasses or contact lenses, making it a lifesaving option for many individuals. Understanding how these elements coalesce enhances our capacity to evaluate LASIK’s role in contemporary eye care.
The Science Behind LASIK


Understanding the science that underlies Laser Assisted In Situ Keratomileusis is crucial to grasp the intricacies of the procedure. This segment connects basic physiological concepts and cutting-edge technology to the outcomes achieved in vision correction. An appreciation for how these elements synergize elucidates the significance of LASIK in modern ophthalmology. With a deeper understanding, patients and professionals alike can make informed decisions regarding eye care.
Understanding the Eye's Anatomy
The eye is a complex organ, designed to convert light into neural signals for visual processing. Its essential components include the cornea, lens, and retina. The cornea, a transparent layer at the front, has a pivotal role in focusing light. It accounts for approximately 70% of the eye’s total optical power. Behind the cornea lies the lens, which further adjusts the light focus onto the retina.
This anatomy is paramount in LASIK surgery. By modifying the corneal shape, LASIK directly influences how light refracts through the eye. A thorough knowledge of eye anatomy is fundamental for practitioners to accurately assess the type of refractive error a patient may have—whether it be myopia, hyperopia, or astigmatism.
Mechanisms of Light Refraction
Light refraction is the bending of light as it passes through different mediums. In the context of human vision, refraction is essential for directing light to the photoreceptors located in the retina. When the eye's optics are misaligned, images become blurred. The LASIK procedure aims to correct this misalignment by reshaping the cornea.
In LASIK, the excimer laser precisely removes microscopic layers of corneal tissue. The desired curvature is achieved to allow light rays to focus directly on the retina. This reshaping not only restores clear vision but can also minimize dependency on corrective lenses—offering an enhanced quality of life for many patients.
Principles of Laser Technology in Surgery
Lasers play a vital role in the efficiency and precision of LASIK. The excimer laser operates using a process called ablative photodecomposition. This technique breaks molecular bonds in the corneal tissue without damaging surrounding areas.
The key features of excimer laser technology include:
- Precision: The laser enables accurate removal of corneal tissue, customized to each patient's specific measurements.
- Speed: LASIK procedures typically last around 15 minutes per eye, minimizing discomfort.
- Safety: Advances in laser technology have decreased risks significantly, leading to high success rates and patient satisfaction.
"Technological advancements in laser systems have transformed LASIK into a reliable method to correct refractive errors."
These principles highlight how the integration of scientific knowledge and technological advancements make LASIK a pioneering approach to treating vision impairment. As research continues, it is expected that future developments in laser technology may further enhance procedure outcomes and patient experiences.
Preoperative Assessment
Preoperative assessment is a critical step in the LASIK process. Its purpose is to gather comprehensive information about the patient’s eye health and overall medical history. This phase ensures that surgery is tailored to the individual needs of each patient, enhancing the likelihood of a successful outcome.
A meticulous evaluation reduces risks and provides clarity on whether LASIK is the right choice. Various factors are considered, including corneal thickness, the degree of refractive error, and overall eye health. Recognizing specific contraindications is essential for patient safety.
Patient Evaluation and Selection
Patient evaluation encompasses a review of both medical and ocular history. Understanding past illnesses or ongoing conditions helps in identifying any underlying risks associated with LASIK. Each candidate undergoes discussions about their visual expectations, which aids the surgeon in making informed decisions.
To ensure optimal results, surgeons also assess age, lifestyle, and occupation during selection. These criteria directly relate to demands placed on one’s vision post-surgery.
Proper selection is vital as it shapes the effectiveness of the LASIK procedure and the satisfaction of the patient long-term.
Diagnostic Examinations
Diagnostic examinations play a key role in the preoperative process. They provide a detailed analysis of the patient's eyes. Two significant tests are corneal topography and wavefront aberrrometry, which assess the unique characteristics of each patient’s vision. Both tests help in formulating a surgical plan.
Corneal Topography
Corneal topography evaluates the anterior surface of the cornea. This detailed mapping is crucial because it identifies irregularities in corneal shape that could affect surgery outcomes.
- Key Characteristic: Its ability to create a three-dimensional map of the cornea makes corneal topography a popular choice.
- Unique Feature: The device captures subtle variations in elevation, allowing for precise planning in LASIK procedures.
- Advantages: It enhances customized approaches to treatment, improving visual results while decreasing complications.
However, limitations do exist. If not correctly interpreted, findings could lead to inappropriate surgical plans.
Wavefront Aberrometry
Wavefront aberrrometry provides a comprehensive analysis of how light is refracted by the eye. This technology helps detect higher-order aberrations that other tests may miss.
- Key Characteristic: It assesses the entire optical system of the eye, offering a complete picture of visual function.
- Unique Feature: This type of measurement focuses on the way light passes through the eye, analyzing it before and after corrective surgery.
- Advantages: Wavefront-guided LASIK can produce superior visual outcomes by correcting unique visual errors.
On the downside, this technology can be more expensive and may not be available in all facilities.


The LASIK Procedure
The LASIK procedure holds a central place in this exploration of Laser Assisted In Situ Keratomileusis. It symbolizes the culmination of various advancements in refractive surgery. This section informs readers about the techniques involved, the duration of the procedure, and the overall experience for patients undergoing LASIK. A clear understanding of these elements is crucial as it aids potential candidates in making informed decisions regarding their vision correction options.
Surgical Techniques Involved
Understanding the surgical techniques used in LASIK is essential for grasping how the procedure achieves its remarkable results. The LASIK procedure generally comprises two main components: flap creation and excimer laser application.
Flap Creation Techniques
Flap creation is a critical aspect of the LASIK procedure. It involves the generation of a corneal flap that provides access to the underlying tissue for laser reshaping. There are primarily two methods for creating this flap: the microkeratome and femtosecond laser techniques.
The microkeratome technique uses a precise surgical blade to create the flap. Its key characteristic lies in its historical significance, being one of the first methods employed in LASIK. It is still regarded as a popular choice due to its efficiency and speed. However, it comes with some disadvantages, such as a potential increase in the risk of complications due to its mechanical nature.
The femtosecond laser, meanwhile, employs laser technology to generate the flap. This technique is favored for its precision and safety. It minimizes the risk of incisions going too deep or causing unwanted side effects. The unique feature of femtosecond laser technology is its ability to customize flap thickness, providing a tailored approach to individual needs.
Excimer Laser Application
Excimer laser application is the next crucial step in the LASIK procedure. This laser is responsible for reshaping the cornea by removing microscopic amounts of tissue, thereby altering the eye's refractive power. It is characterized by its ability to deliver highly targeted, precise ablation with minimal thermal effect on surrounding tissues, enhancing safety and recovery.
The excimer laser is popular due to its versatility; it can treat a variety of refractive errors such as myopia, hyperopia, and astigmatism. Its unique feature includes the use of wavefront-guided technology, which enables personalized treatment based on a patient’s specific corneal irregularities. However, while the benefits are substantial, some potential risks include aberrations and dry eye symptoms post-surgery.
Duration and Experience of the Procedure
The LASIK procedure typically lasts about 15 to 30 minutes per eye. This brief duration belies the intricate planning and preparation that precedes the actual surgery. Patients often experience minimal discomfort, with many reporting an immediate improvement in their vision upon completion.
During the procedure, a calming atmosphere is maintained. Patients remain awake, allowing for real-time adjustments based on their feedback. Following the operation, most patients can resume normal activities within a day or two, although complete recovery might take a little longer.
Overall, the LASIK experience blends technology with personal care, providing individuals with the chance to enhance their vision rapidly and effectively.
Benefits of LASIK
Laser Assisted In Situ Keratomileusis (LASIK) has become a leading option for those seeking correction for refractive errors. Its significance is rooted in the transformative potential it offers for visual clarity. Not only does LASIK provide a practical solution for conditions such as myopia, hyperopia, and astigmatism, it fundamentally changes how patients experience their daily lives. The advantages of this procedure are manifold.
Visual Outcomes and Success Rates
The primary allure of LASIK lies in its impressive visual outcomes. Clinical studies show that approximately 96% of patients achieve 20/25 vision or better after the procedure. These results often exceed patients’ expectations, leading to a high rate of satisfaction.
Success rates are largely attributable to advancements in technology and methodologies over the years. Notably, bladeless LASIK techniques and wavefront-guided LASIK have improved precision, allowing for more individualized treatment plans. The reliability of the excimer laser technology further enhances the predictability of outcomes, making LASIK a top choice among refractive surgeries.
"LASIK not only corrects vision but allows individuals to reclaim everyday activities without the need for glasses or contact lenses."
Studies indicate that complications are rare. While some patients may experience temporary side effects like dry eyes or glare, these are often manageable and resolve over time. Continuous follow-up studies show that the benefits generally outweigh potential risks, solidifying LASIK’s reputation as a safe and effective procedure.
Quality of Life Improvements
Beyond visual enhancement, LASIK contributes significantly to improved quality of life. The freedom from corrective lenses is transformative; patients often report increased convenience and an active lifestyle. Everyday activities, such as swimming or exercising, are more accessible without the constant concern of losing or breaking glasses.
Many patients also experience psychological benefits. The gain in visual acuity boosts confidence and self-esteem, impacting both personal and professional spheres positively. For example:
- Employment Opportunities: Clear vision can open doors to career advancement by meeting the visual requirements of specific jobs or improving work efficiency.
- Social Interaction: Improved vision often leads to greater social engagement as patients feel more comfortable in various settings.
Risks and Complications
Understanding the risks and complications associated with Laser Assisted In Situ Keratomileusis (LASIK) is critical for patients considering the procedure. Awareness of these factors helps individuals make informed decisions about their eye health. LASIK, while generally safe and effective, is not without its potential drawbacks.
Common Postoperative Issues


Postoperative issues can arise after LASIK surgery, even in patients who are ideal candidates. Some common problems include:
- Dry Eyes: This is one of the most frequently reported issues after LASIK. Patients may experience a decrease in tear production, leading to sensations of dryness and discomfort.
- Visual Disturbances: Some patients notice glare, halos, or starbursts around lights, especially at night. These disturbances can vary in intensity.
- Flap Complications: The creation of the corneal flap is central to LASIK. Issues such as improper flap position or wrinkles can occur but are usually correctable.
- Infection: Although rare, infections can develop post-surgery. It highlights the importance of adhering to postoperative care recommendations.
Most of these issues tend to resolve within a few weeks to months. Regular follow-up with healthcare professionals is important to monitor and address any concerns promptly.
Long-term Risks Associated with LASIK
While many patients experience improved vision post-LASIK, some long-term risks exist:
- Regression: In certain cases, the eye may regress towards its pre-surgical prescription over time. This could necessitate an enhancement procedure or other corrective measures.
- Corneal Ectasia: This is a rare condition where the cornea becomes progressively thinner and bulges forward. It can lead to significant vision problems and may require additional treatments, such as corneal cross-linking or even a corneal transplant.
- Loss of Visual Acuity: Some patients report a slight decrease in their best-corrected vision, which could impact daily life or specific activities.
- Chronic Dry Eye: For some individuals, dry eye symptoms can persist long after surgery, affecting comfort and vision quality.
"Though LASIK can significantly improve vision, it is essential to understand that risks and complications, albeit rare, can occur."
For patients considering LASIK, discussing these risks openly with an ophthalmologist is crucial. Understanding personal health factors and individual risks can help ensure the best possible outcomes.
Postoperative Care
Postoperative care is a critical phase in the journey of patients undergoing Laser Assisted In Situ Keratomileusis (LASIK). It ensures the success of the procedure and provides the necessary support for optimal recovery. After surgery, the eyes undergo a healing process, and adequate care can significantly enhance visual outcomes and minimize complications.
The significance of postoperative care can be outlined as follows:
- Healing Support: Postoperative care aids in the natural healing of the cornea. It involves instructions on how to care for the eyes, including the use of prescribed eye drops and protective measures.
- Monitoring Potential Complications: Close observation is essential to recognize and address any complications that may arise early in the recovery process. Early detection can lead to more effective interventions.
- Patient Education: Patients must be educated about what to expect post-surgery. Understanding potential symptoms, like temporary vision fluctuations or discomfort, helps alleviate fears and improves patient compliance with care instructions.
- Long-term Outcomes: Proper care contributes to long-lasting success. Patients who adhere to follow-up protocols often report better visual acuity and satisfaction compared to those who neglect aftercare.
Expected Recovery Timeline
The expected recovery timeline following LASIK can vary widely among patients. However, there are typical stages of recovery that many individuals can anticipate:
- Immediate Postoperative Period (0-24 hours): Many patients experience discomfort, light sensitivity, or a gritty sensation immediately after surgery. Vision may be blurry but usually improves within hours.
- First Week: Most patients can resume routine activities by the next day, but activities that strain the eyes, such as reading or screen time, should be minimized. Follow-up visits in this period help assess recovery.
- One Month: By now, vision should stabilize for the majority of patients. Some may still notice minor fluctuations. This is normal as healing continues.
- Three to Six Months: Most patients achieve their best visual acuity within this time frame. Some may require enhancements or additional prescriptions, particularly if they had pre-existing conditions.
- One Year and Beyond: Long-term follow-up will help ensure that vision remains stable. Regular eye exams are essential for monitoring eye health and ensuring continued success of the surgery.
Follow-up Visits and Monitoring
Follow-up visits are integral to the LASIK postoperative care process. These appointments allow healthcare providers to monitor healing and address patient concerns effectively.
During follow-up visits, the following considerations are typically assessed:
- Visual Acuity Measurement: Checking how well patients see at different distances will help evaluate the success of the procedure quickly.
- Corneal Health Assessment: Instruments like a slit lamp are used to examine the cornea and ensure it is healing well without any abnormalities.
- Addressing Concerns: Patients should feel free to discuss any symptoms, such as dryness, glare, or fluctuating vision, to receive appropriate guidance.
- Adjusting Medications: Eye drops and other medications may be modified based on healing progress and any side effects encountered by the patient.
"Effective postoperative care not only enhances the visual outcomes but also strengthens the patient's confidence in their surgical experience."
The Future of LASIK
The landscape of refractive surgery is continuously evolving, and the future of Laser Assisted In Situ Keratomileusis (LASIK) holds significant promise. Technological advancements and ongoing research will improve patient outcomes and accessibility. With a growing understanding of visual impairments and the dynamics of eye health, the upcoming years are likely to see innovations that enhance LASIK procedures.
Several key elements influence the future of LASIK:
- Safety Improvements: Ongoing research aims to mitigate risk factors inherent in the LASIK procedure.
- Customization of Treatment: Increased precision can be achieved with improved diagnostic tools, allowing for more tailored surgical interventions.
- Broader Patient Eligibility: As techniques advance, more individuals with diverse eye conditions may become suitable candidates for LASIK.
This future perspective not only focuses on improvement in medical technology but also encompasses patient experiences and the overall impact on quality of life. Advancements in LASIK could redefine standards of vision correction.
Technological Advancements
The integration of new technologies into LASIK will fundamentally change how the procedure is performed. Innovations such as wavefront-guided LASIK and femtosecond laser technology are examples of how technology enhances surgical outcomes.
- Wavefront-Guided LASIK: This technique utilizes detailed vision maps generated by wavefront aberrometry. By addressing specific aberrations, the procedure aims to enhance overall visual quality beyond conventional methods.
- Femtosecond Laser Technology: This technology allows for more precise and safe flap creation. Unlike traditional microkeratomes, femtosecond lasers can create thinner corneal flaps, reducing the risk of complications.
These technologies are paving the way for rapid improvements in LASIK surgery. As tech continues to evolve, ongoing research and meaningful innovations will emerge, thus enhancing both effectiveness and safety.
Emerging Alternatives to LASIK
In the quest for optimal vision correction, various alternatives to LASIK are gaining attention. Understanding these alternatives provides valuable context on the evolving choices for patients.
- SMILE (Small Incision Lenticule Extraction): SMILE is a minimally invasive procedure that has shown promise for nearsightedness and astigmatism. It utilizes a femtosecond laser, similar to LASIK, but does not require a corneal flap.
- PRK (Photorefractive Keratectomy): While older than LASIK, PRK remains a viable option. It is suitable for patients with thin corneas. In this procedure, the outer layer of the cornea is removed, and the laser reshapes the underlying tissue directly.
- Refractive Lens Exchange: For presbyopia or severe hyperopia, this surgical procedure replaces the eye’s natural lens with an artificial one. It is an option for those not suitable for LASIK due to high refractive errors.
The emergence of these alternatives is vital for patients, further diversifying options in surgical vision correction. These advancements reflect the shift toward personalized solutions in eye surgery.







